Just a few of the decades of studies about patient monitoring
Randy Durbin, DO, MSPH Vice-President, Medical Affairs & Federal Programs, Karna, LLC
SUMMARY The following represents our analysis of three years of cardiac patient discharge data supplied by an Ascension hospital in Alabama and comprised exclusively of patients affiliated with a single cardiology practice. The purpose of the analysis was to estimate the experience of patients’ hospital admissions (and readmissions within 30 days) before and after participating in a Chronic Care Management (CCM) or Remote Patient Monitoring (RPM) care strategy. Here are the highlights and benefits of Remote Patient Monitoring from our review of discharge data for this patient cohort.
METHOD This patient cohort consisted of existing cardiac patients who initially had at least one prior hospitalization attributable to their underlying cardiac condition. This sets the context that this cohort was comprised of sick patients. The patients that were offered additional surveillance via CCIQ (“Intervention Cohort”), were by definition, part of the sickest 15% of cardiac patients that make up 85% of system costs for cardiac care (hospital, specialists, pharmacy).
Using crude analysis of differences in admissions over time, there seemed to be up to a 29% reduction in all-types hospital admissions from one year to the next after the initiation of CCM. After adjusting for short-term admissions based on scheduled procedures and using the most conservative rules for inclusion, there was still over an 8% reduction in hospital admissions in this group that underwent CCM.
FINDINGS Several likely implications of the analysis of this CCM strategy including key benefits of Remote Patient Monitoring for cardiac patients.
1: AMI Admission Cost Data AHRQ (2012) https://www.hcup-us.ahrq.gov/reports/projections/2012-02.pdf
2: CHF Admission Cost Data Published online 2017 May 10. doi: 10.2147/RMHP.S130341
3: Readmission Cost Data JAMA. 2017;317(5):530-531. doi:10.1001/jama.2016.20468
Isabelle Vedel, MD, PhD and Vladimir Khanassov, MD, MSc . Transitional Care for Patients With Congestive Heart Failure: A Systematic Review and Meta-Analysis. Ann Fam Med November/December 2015 vol. 13 no. 6 562-571. doi: 10.1370/afm.1844
PURPOSE We aimed to determine the impact of transitional care interventions (TCIs) on acute health service use by patients with congestive heart failure in primary care and to identify the most effective TCIs and their optimal duration.
METHODS We conducted a systematic review and meta-analysis of randomized controlled trials, searching the Medline, PsycInfo, EMBASE, and Cochrane Library databases. We performed a meta-analysis to assess the impact of TCI on all-cause hospital readmissions and emergency department (ED) visits. We developed a taxonomy of TCIs based on intensity and assessed the methodologic quality of the trials. We calculated the relative risk (RR) and a 95% confidence interval for each outcome. We conducted a stratified analysis to identify the most effective TCIs and their optimal duration.
RESULTS We identified 41 randomized controlled trials. TCIs significantly reduced risks of readmission and ED visits by 8% and 29%, respectively (relative risk = 0.92; 95% CI, 0.87–0.98; P = .006 and relative risk = 0.71; 95% CI, 0.51–0.98; P = .04). High-intensity TCIs (combining home visits with telephone followup, clinic visits, or both) reduced readmission risk regardless of the duration of follow-up. Moderate-intensity TCIs were efficacious if implemented for a longer duration (at least 6 months). In contrast, low-intensity TCIs, entailing only followup in outpatient clinics or telephone follow-up, were not efficacious.
CONCLUSIONS Clinicians and managers who implement TCIs in primary care can incorporate these results with their own health care context to determine the optimal balance between intensity and duration of TCIs. High-intensity interventions seem to be the best option. Moderate-intensity interventions implemented for 6 months or longer may be another option.
Hang Ding; Mohan Karunanithi; Yogi Kanagasingam; Janardhan Vignarajan and Yuben Moodley. A pilot study of a mobile-phone-based home monitoring system to assist in remote interventions in cases of acute exacerbation of COPD. Journal of Telemedicine and Telecare. 2014; 20(3): 128–134.
Summary
We conducted a six-month feasibility study of a mobile-phone-based home monitoring system, called M-COPD. Patients with a history of moderate Acute Exacerbation of COPD (AECOPD) were given a mobile phone to record major symptoms (dyspnoea, sputum colour and volume), minor symptoms (cough and wheezing) and vital signs. A care team remotely monitored the recorded data and provided clinical interventions. Eight patients (mean age 65 years) completed the trial. Ten acute exacerbations occurred during the trial and were successfully treated at home. Prior to the AECOPD episode, the combined score of the major symptoms increased significantly (P<0.05). Following the intervention, it decreased significantly (P<0.05) within two weeks and returned to the baseline. The score of the minor symptoms also increased significantly (P<0.05), but the decrease following the intervention was not significant. There were significantly fewer hospital admissions during the trial, fewer ED presentations and fewer GP visits than in a six-month matched period in the preceding year. The results demonstrate the potential of home monitoring for analyzing respiratory symptoms for early intervention of AECOPD.
Elizabeth Madigan, PhD, RN, FAAN, Brian J. Schmotzer, MS, Cynthia J. Struk, PhD, MSN, BSN, Christina M. DiCarlo, MD, George Kikano, MD, Ileana L. Piña, MD, MPH, and Rebecca S. Boxer, MD, MS. Home Health Care With Telemonitoring Improves Health Status for Older Adults with Heart Failure. Home Health Care Serv Q. 2013; 32(1): 57–74. doi: 10.1080/01621424.2012.755144
Abstract
Home telemonitoring can augment home health care services during a patient’s transition from hospital to home. Home health care agencies commonly use telemonitors for patients with heart failure although studies have shown mixed results in the use of telemonitors to reduce rehospitalizations. This randomized trial investigated if older patients with heart failure admitted to home health care following a hospitalization would have a reduction in rehospitalizations and improved health status if they received telemonitoring. Patients were followed up to 180 days post-discharge from home health care services. Results showed no difference in the time to rehospitalizations or emergency visits between those who received a telemonitoring vs. usual care. Older heart failure patients who received telemonitoring had better health status by home health care discharge than those who received usual care. Therefore for older adults with heart failure telemonitoring may be important adjunct to home health care services to improve health status.
Catherine Klersy, MD, MSc; Annalisa De Silvestri, MSc; Gabriella Gabutti, MA; François Regoli, MD; Angelo Auricchio, MD. A Meta-Analysis of Remote Monitoring of Heart Failure Patients. J Am Coll Cardiol. 2009; 54(18): 1683-1694. doi:10.1016/j.jacc.2009.08.017
Objectives The purpose of this study was to assess the effect of remote patient monitoring (RPM) on the outcome of chronic heart failure (HF) patients.
Background Remote Patient Monitoring (RPM) via regularly scheduled structured telephone contact between patients and health care providers or electronic transfer of physiological data using remote access technology via remote external, wearable, or implantable electronic devices is a growing modality to manage patients with chronic HF.
Methods After a review of the literature published between January 2000 and October 2008 on a multidisciplinary heart failure approach by either usual care (in-person visit) or remote patient monitoring RPM, 96 full-text articles were retrieved: 20 articles reporting randomized controlled trials (RCTs) and 12 reporting cohort studies qualified for a meta-analysis.
Results Respectively, 6,258 patients and 2,354 patients were included in RCTs and cohort studies. Median follow-up duration was 6 months for RCTs and 12 months for cohort studies. Both RCTs and cohort studies showed that RPM was associated with a significantly lower number of deaths (RCTs: relative risk [RR]: 0.83, 95% confidence interval [CI]: 0.73 to 0.95, p = 0.006; cohort studies: RR: 0.53, 95% CI: 0.29 to 0.96, p < 0.001) and hospitalizations (RCTs: RR: 0.93, 95% CI: 0.87 to 0.99, p = 0.030; cohort studies: RR: 0.52, 95% CI: 0.28 to 0.96, p < 0.001). The decrease in events was greater in cohort studies than in RCTs.
Conclusions Remote Patient Monitoring RPM confers a significant protective clinical effect in patients with chronic HF compared with usual care.
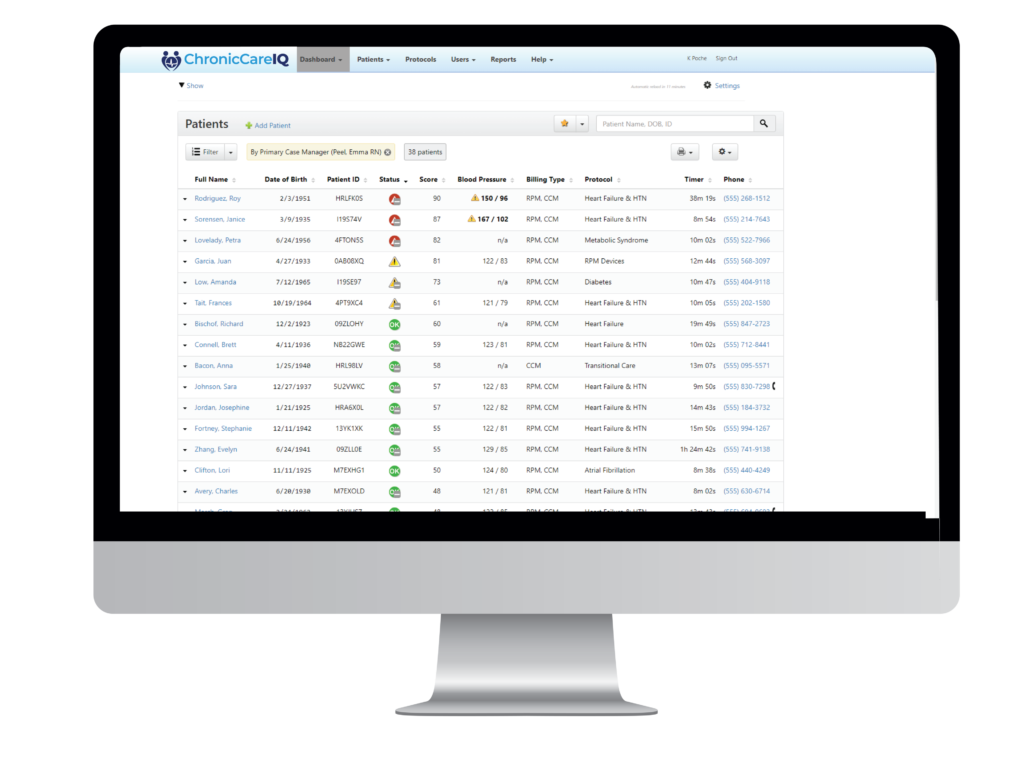
See for yourself how we can help you grow without adding more resources or risk.
Now is the time to explore a better care management solution that gives you confidence to grow your practice while giving patients confidence in managing their complex conditions.
© 2024 ChronicCareIQ, All rights reserved