When your behavioral health patients need extra attention and even psychiatric services, the care coordination activities between primary and behavioral healthcare professionals qualify for reimbursement.
The complexity, variety and frequency of behavioral health treatments place high demands on practices and often requires interaction with psychiatric specialists.
And as the medical community continues to advance its understanding of the tight connection between a patient’s mental and physical health, CMS is encouraging the integration of behavioral health with primary care through the BHI and CoCM codes that support collaboration and coordination among each discipline.
The result? Patients get access to the care they need to stay on track while you get reimbursed properly for the time you take to coordinate behavioral health services and medications.
"Gaining insights and guidance from primary care physicians can sometimes be challenging. When our primary care partners are using ChronicCareIQ, it's much easier for us to stay connected and informed while also making sure each care team member is reimbursed properly."
Psychiatrist, Independent Behavioral Health Practice
Once patients are enrolled in your care management program, the system begins to proactively engage with them according to the clinical protocols you set for their specific chronic conditions. Engagement comes in the form of a series of simple questions that patients respond to – either on their phone, tablet, or personal computer.
As your team provides care and supportive services, such as phone calls, coordinating medication refills, and speaking with specialists, the system recognizes those interactions and automatically captures and timestamps each activity. Each eligible activity is then assigned the appropriate care management program codes. There is no need for staff to manually provide documentation or follow reimbursement guidelines for hitting certain thresholds – the system does the work for them.
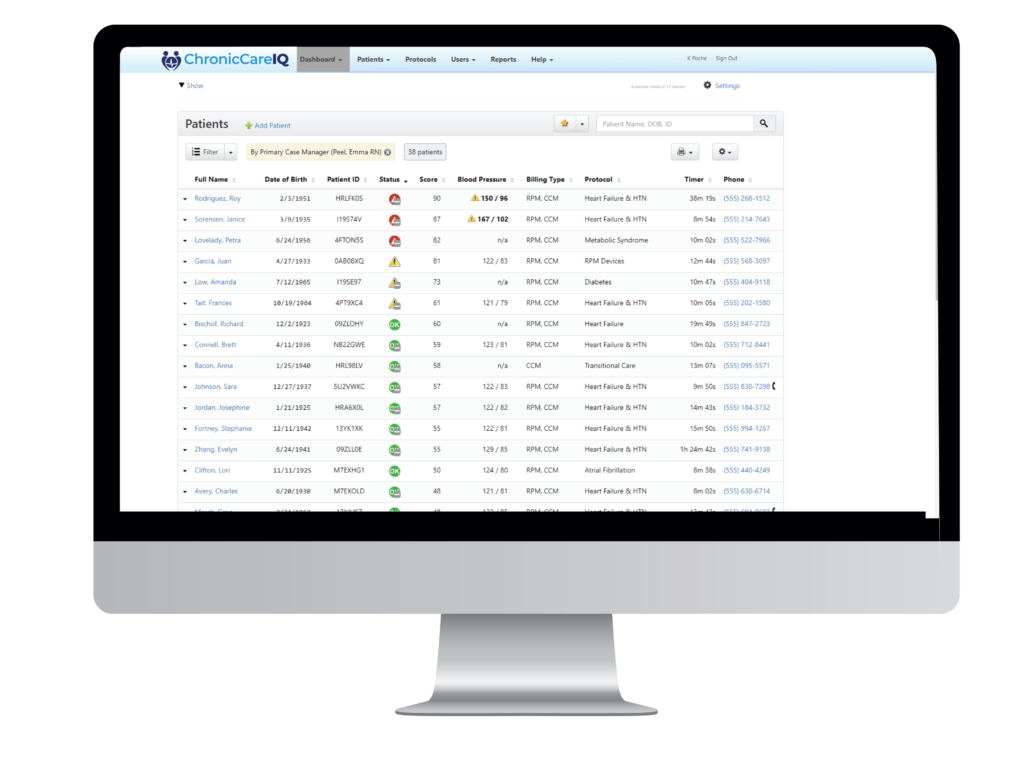
Your clinical team members simply review their red-yellow-green dashboards to know which patients are at risk for falling out of the guidelines you’ve set and which ones need immediate attention. They can drill down to the details of each patient, review recent interactions and see the latest data coming in from patients and/or monitoring devices. This gives them a complete picture of the patient in real-time so they can make more informed decisions about what needs to happen for each patient.
Your back-office staff has access to reports that show which clinical activities were performed on which patients so preparing claims for reimbursement is simple. The system even tells them how close each enrolled patient is to fulfilling the respective CCM requirements each month.
© 2024 ChronicCareIQ, All rights reserved