By Juli Eschenbach, Custom Solutions Manager and Clinical SME
The Centers for Medicare & Medicaid Services (CMS) delighted care management teams and advocates with the published 2026 Medicare Physician Fee Schedule (PFS) FINAL Rule on Nov 5, 2025. The final 2026 changes for Remote Patient Monitoring (RPM) are significant and we are very excited that CMS is moving RPM into the mainstream of patient care.
In addition to new proposed RPM codes, CMS made it clear they will continue to support behavior health with new Advanced Primary Care Management (APCM) add-on codes for Behavioral Health Integration (BHI) — with an emphasis on integrating BHI more heavily into the other care management spaces.
Federally Qualified Health Health Center (FQHC) will also benefit from the focus on behavior health and will be transitioned to PFS code billing for BHI services during 2026.
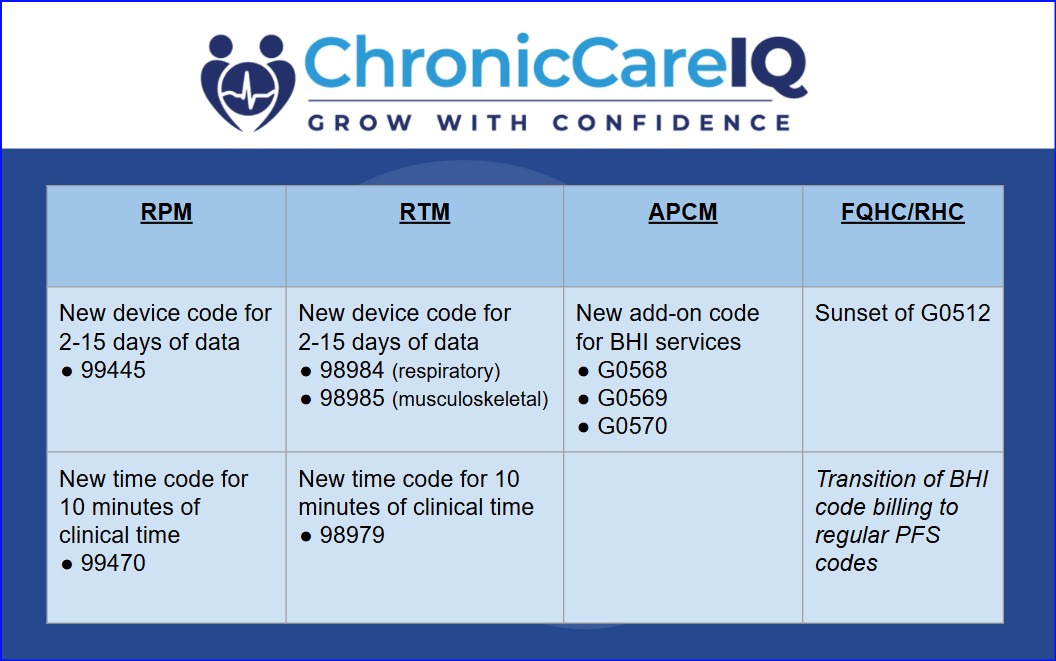
Here is an overview of the CMS Final Rule 2026 exciting new changes for Care Management:
CMS finalized new codes for fewer monitoring days and shorter time requirements. This means that clinical care for these patients is recognized at a broader level:
CMS has kept existing RPM device code 99454 to cover 16 to 30 days of readings in a 30-day period and RPM time. They also keep existing RPM time codes 99457 and 99458, which cover increments of 20 minutes.
What does this mean? CMS emphasizes the importance of physiologic data and the value of remote care time spent to patient care and indicates it aims to protect reimbursements in this area. CMS also clarified that they see RPM as a “longitudinal service” that should continue as long as it is medically necessary with practice dispensed devices.
In an expansion of services covered in last year’s new APCM codes, CMS has created an add-on code to APCM specific to BHI services. This allows providers to bill for service for BHI by interdisciplinary teams complimentary to APCM, without the requirement of time tracking.
CMS is underscoring the value of RTM care time spent and data input from patients for non-physiologic patient data the addition of three new codes:
Remote Therapeutic Monitoring time codes and device codes are going to be fully available as part of the suite of services ChronicCareIQ supports in 2026. Please contact our support for more information about the requirements for these codes.
CMS is sunsetting the FQHC/RHC code G0512 and converting billing to the PFS equivalent codes. This was the case in 2025 for G0511, and will occur in the same manner. FQHC/RHCs also qualify for add-on codes proposed for BHI services under the APCM umbrella, expanding the care management billing opportunities to some of the most vulnerable populations.
Our process for integrating annual code updates is meticulous and ensures accuracy and compliance:
We will share specific information about how ChronicCareIQ adds these game-changing codes to our software:
We appreciate your excitement and patience as we work diligently to ensure a seamless, compliant, and feature-rich transition into the new 2026 codes.
ChronicCareIQ is with you every step of the way to support and advise on regulatory changes big and small. For ongoing guidance, connect with us on social media here.